Engineered T-cell therapies are redefining cancer treatment by transforming the immune system into a precision therapeutic tool. Through genetic engineering, a patient’s own T-cells are modified to recognize tumor-specific antigens, enabling targeted destruction of cancer cells that once evaded immune detection. This approach marks a major advance for treating cancers such as ovarian cancer, where conventional therapies often fall short.
However, this scientific progress brings forth ethical consideration about who will benefit from these innovations. There are many high costs associated with engineered cell therapies that raise questions about its accessibility and whether only patients with the financial means can receive them. Additionally, ensuring fair access to these life-saving T-cell therapies becomes not only a scientific but also a moral responsibility.
Ovarian cancer remains a major threat to women’s health, primarily in older women. According to the American Cancer Society, about 21,000 women are affected by ovarian cancer and about 13,000 women die from it. A woman’s risk of getting ovarian cancer during her lifetime is about 1 in 91, signifying the need for effective treatment options. This troubling statistic highlights the ethical pressure of innovating while still maintaining patient safety. Researchers aim to avoid rushing the adoption of new therapies before their long-term effects are fully understood to ensure that hope for new treatments does not overpower caution. Within this ethical framework, emerging approaches such as engineered T-cells demonstrate how medicine is shifting towards highly adaptive strategies against cancer by merging immunology with molecular design.
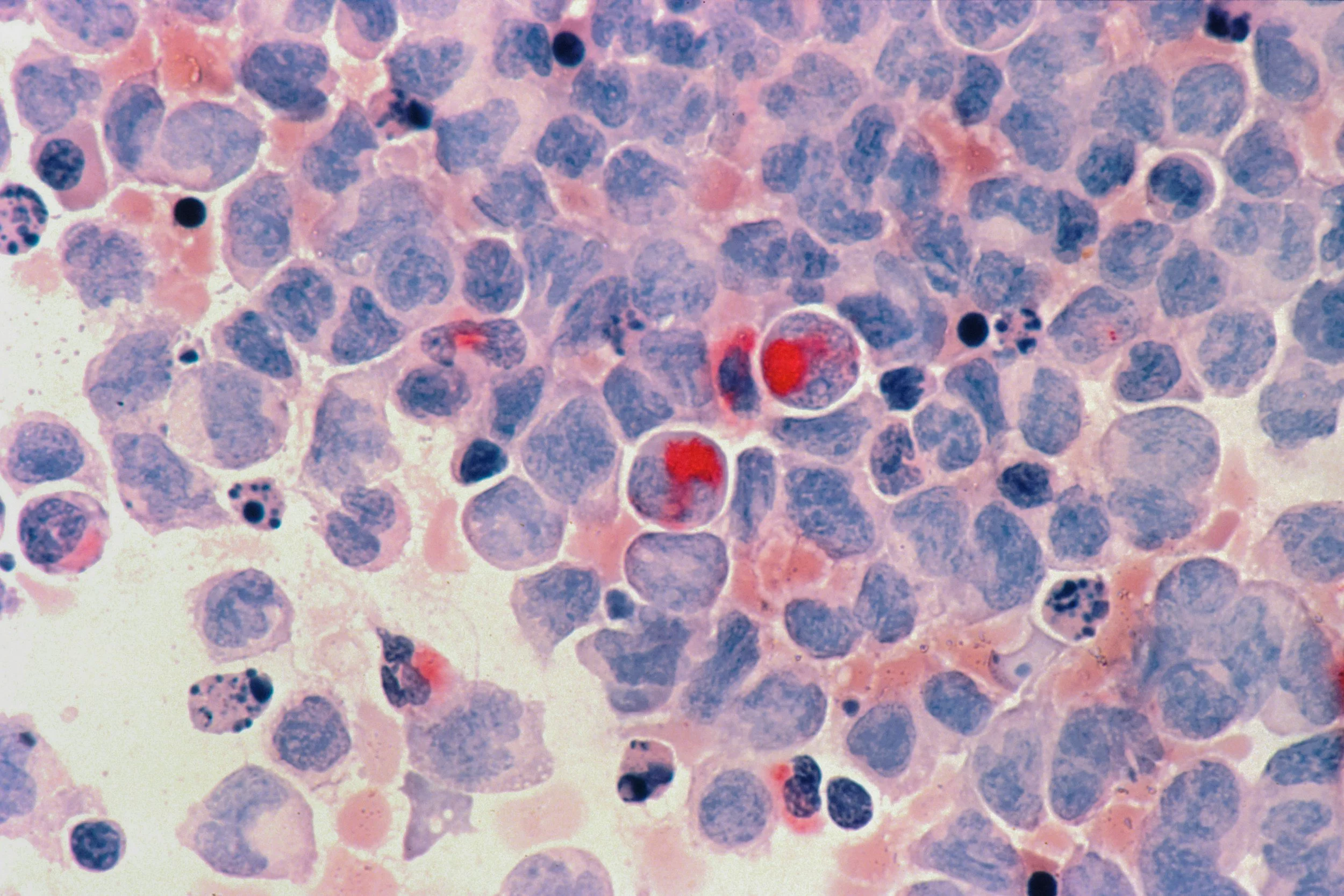
To understand how these therapies achieve such precision, it’s essential to examine how engineered T-cells are created and reprogrammed. T-cells are the backbone of CAR-T cell therapy. Engineered T-cells begin by collecting blood from the patient and separating out the T-cells. Once harvested, the T-cells can be genetically engineered in a lab to produce proteins on their surfaces called chimeric antigen receptors, otherwise known as CARs. CARs help the cells adhere to specific proteins called antigens that are present on cancer cells as well as enhancing the T-cells ability to kill cancer cells. The modified T-cells are then grown until there are millions of them and are then infused back into the patient. After the infusion, the engineered T-cells continue to expand in the patient’s body and kill any cancer cells that have the antigen on their surfaces. However, because these therapies involve this genetic modification, patients must be fully informed that their immune systems are being altered and must provide consent. This raises ethical concerns about ensuring patients are fully informed of both the potential benefits of these treatments and the irreversible nature of these biological interventions. In engineering and training T-cells to act with such precision, scientists and researchers are not only reshaping cancer therapy–they are redefining the boundaries between natural immunity and engineered biology.
Despite their precision, engineered T-cells must overcome the hostile environment of ovarian tumors, shielding malignant cells from immune detection and attack. Ovarian cancer is one of the most lethal gynecological malignancies due to its ability to resist treatment and immune evasion.
Current CAR-T cell therapies have had challenges and limited success against ovarian cancer due to its immunosuppressive environment. Ovarian cancer reduces the efficacy of CAR-T cell therapy because the tumor microenvironment induces cellular stress in T-cells; it was found that ovarian tumors can suppress the production of Transgelin 2 in T-cells due to this stressful environment. To solve this problem, researchers tried to insert a modified Transgelin 2 gene that can’t be suppressed by the tumor’s stressful microenvironment so that it continues to be expressed. This solution raises ethical concerns about how far biology can be altered and where the line is between healing disease and redesigning cells beyond limit. This manipulation must be carefully modified to ensure that enhancing immune strength doesn’t lead to further genetic consequences. The modified T-cells are more effective at attacking ovarian tumors than normal CAR-T cells, suggesting improved strategies for enhancing the efficacy of T-cell immunotherapies in hostile tumor environments.
Engineered T-cell therapies have sparked new hope in the fight against ovarian cancer, but their progress from experiments to effective clinical therapies has faced significant challenges that researchers continue to work to overcome. Further advances for CAR-T cell therapies in ovarian cancer are continuing to be developed and focus on improving effectiveness against solid tumors. Researchers have found that combining oncolytic viruses with CAR-T cells have been shown to enhance CAR-T cell migration into the tumor, strengthening their activity. Scientists are also researching the use of nanotechnology with CAR-T cell therapy in creating new treatments of solid tumors.
However, these advances in biotechnologies introduce ethical complexity that increases potential benefits as well as potential harm which requires long-term patient monitoring to protect them from unintended side effects. Despite progress of CAR-T cell therapies, challenges still present themselves including the tumor’s immunosuppressive environment and the engineered T-cells may lose their effectiveness over time. To overcome these challenges, researchers are exploring reducing the activity of immunosuppressive cells in the tumor, making CAR-T cells target multiple tumor markers, and integrating other therapies in combination with CAR-T therapy. As more advances in overcoming ovarian cancer presents itself, it’s the responsibility of these researchers to ensure that progress is never prioritized over ethical reflection.
Ovarian cancer poses a significant threat to women’s health and researchers continue to develop advancements in therapies that can be effectively applied in clinical settings. Future advancements and innovations further enhance the development of CAR-T cell therapies in treating ovarian cancer.
Although many challenges remain, ongoing research and technological advances suggests that CAR-T cell therapy may achieve significant breakthroughs in treating ovarian cancer. As advances progress, it is crucial to ensure that ethical principles evolve alongside scientific innovations, so that patient well-being is enforced and access to therapies are available to all. With continued research guided by strong ethical principles, engineered T-cell therapies have the potential not only to progress cancer treatment, but to also set a new standard for ensuring that progress serves humanity as a whole.