The Problem
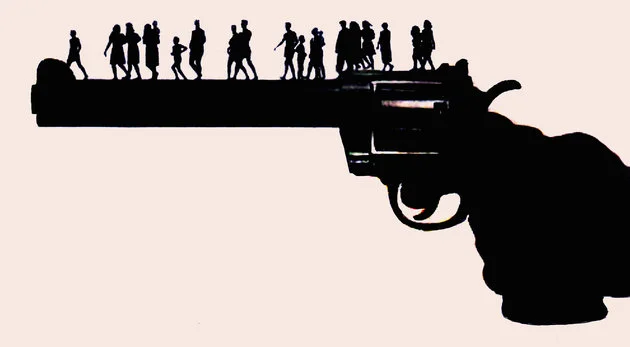
Unintentional injuries and violence are among the leading causes of death, hospitalization, and disability in Virginia. Typical culprits on the top of that list are motor vehicle accidents, accidental gun deaths, and poisonings. In 2014, however, trends began to change.
For the first time in the state’s history, fatal drug overdose is now the number one method of unnatural death in the Commonwealth. It killed 986 people in 2014, eclipsing both motor vehicle-related fatalities and gun-related deaths.1
This new reality mimics trends in opioid and heroin addiction nationally. Also in 2014, more Americans died of drug overdoses than any other year on record, accounting for more than 47,000 total deaths.2 While a significant percentage of these deaths are a result of heroin overdoses, over half are related to opioid-based prescription painkillers, such as oxycodone, fentanyl, hydrocodone, or methadone.3
Oxycodone, fentanyl, and heroin are the most common painkillers seen on the streets today. Historically, oxycodone has been the number one prescribed drug to cause opioid overdose. However in recent years, fentanyl, which is up to 100 times more potent than morphine, has surpassed it.4
This is due to the fact that fentanyl is being illicitly produced instead of pharmaceutically produced. This illicit form of fentanyl is produced by international drug traffickers who import the drug into the United States and often mix it into heroin being sold. According to the Virginia Department of Health (VDH), by late 2013 and early 2014, some heroin being sold on the street was actually completely fentanyl, unbeknownst to the user.1
This illicitly produced fentanyl, especially fentanyl mixed with heroin, has been the biggest contributor to the significant increase in the number of fatal opioid overdoses in Virginia.
Source: Virginia Department of Health1
The Response
The rise of this epidemic has understandably caught the attention of policy leaders, law enforcement officials, and healthcare professionals alike. In typical government fashion, taskforces were formed, workgroups convened, and coalitions established.
Virginia Governor Terry McAuliffe created the Governor’s Task Force on Prescription Drug and Heroin Abuse in the beginning of 2015. The Task Force was directed to provide a range of policy recommendations, including how to: (1) raise public awareness about the misuse of prescription painkillers, (2) train health care providers on best practices for pain management, (3) identify treatment options and alternatives to incarceration for people with addiction, and (4) promote the safe storage and disposal of prescription drugs.3
The enforcement of these recommendations is currently underway across the state and many players are involved. State agencies, academics, law enforcement, and health care providers are forming partnerships and collaborating with each other in order to do their due diligence.
As an example, the Virginia Department of Medical Assistance Services (DMAS) worked with the Department of Behavioral Health and Developmental Services (DBHDS) to increase access to treatment for Virginia’s Medicaid members by increasing Medicaid reimbursement rates for addiction services.5
The new rates go into effect in April 2017 and increase some payments up to 400 percent. In preparation for the big change, DMAS, DBHDS, and VDH have also partnered together to host statewide trainings for medical providers, behavioral health providers, and administrative professionals. The trainings will raise awareness about the new reimbursement structure as well as educate providers on how to implement evidence-based addiction management services into their practice.
Medication addiction treatment, otherwise referred to as MAT, is one of these evidence-based treatments. MAT combines continuous behavioral counseling with anti-addiction medicines like buprenorphine or Suboxone in order to address the physical, mental, and social factors of addiction. Suboxone, which is a synthetic mix of buprenorphine and the overdose reversal drug naloxone, suppresses opioid cravings, decreases withdrawal symptoms, and is proven to help addicts recover from their illness. A study conducted by the National Institute on Drug Abuse (NIDA) found that Suboxone reduced prescription painkiller abuse in nearly half of all participants.6
With the new payment incentives and increased education and trainings for MAT, Virginia will undeniably see an increase in the number of providers that offer fully comprehensive services. As a result, low income populations who are most disproportionately affected by the substance use epidemic will have improved access to community-based addiction treatments that promote full integration of physical health and traditional mental health services.
Counties are also working at the local level to carry out some of the Governor’s recommendations. According to Loudoun Emergency Medical Services (EMS), in 2015 Loudoun County had a total of 35 suspected heroin overdoses and since January 2016, there have been 71 overdose incidents recorded, 30 of which appeared to involve an opiate.
Loudoun County Police Department drug drop off box
For years, local county and town law enforcement agencies have participated in biannual Drug Take Back Days. These events have resulted in disposal of almost 8,000 pounds of unneeded prescriptions, but the Loudoun County Health Council recognized the need for disposal locations that offered continuous access throughout the year.
Drug collection boxes provide a safe way for residents to dispose of prescription drugs without cost to them. The local Health Department sought and received a grant from the CVS Pharmacy and the Partnership for Drug-Free Kids to increase the number of drug drop off boxes from one to now five sprinkled throughout the county.
The drug collection boxes give citizens the opportunity to remove as many unused or expired prescription drugs as possible and are another evidence-based approach to prevent further drug abuse and drug overdoses in the community.
Worry in Southwest
In light of the great work being done by these state and local agencies, there still remain some skeptics about the impact and effectiveness of medication assisted treatment for opioid addiction.
Despite the fact that Suboxone is not supposed to produce a narcotic high, users who snort or inject it, or combine it with benzodiazepines or alcohol, report being able to achieve similar euphoric effects of heroin or strong prescription painkillers.
In fact, towns in rural southwest Virginia describe Suboxone as a “menace” to their community.7 According to an article in the Culpepper Star Exponent, “Suboxone is the most-abused, most-sought-after street drug across that part of the state.” Law enforcement officials are increasingly concerned that people are using the drug to help feed their addictions instead of cure them.
However, experts believe it is likely that in southwest Virginia the availability of Suboxone has been perpetuated from cash clinics that don’t typically offer the comprehensive evidence-based treatment that addicts need to be successful. Behavioral counseling is an integral part of MAT and people abusing Suboxone may not be receiving the full spectrum of care, either due to access issues, financial barriers, psychosocial neglect, or a multitude of other reasons.
While the dangers and abusive potential of Suboxone are indeed a reality for many people in the region, policymakers in Virginia and in Washington, DC remain strong proponents of MAT if executed correctly. President Obama’s 2017 proposed budget includes $1 million for expansion of MAT, and Virginia is expected to receive federal funding to match its $11 million dedicated to fighting the opiate epidemic.7
The access and availability of MAT will certainly increase as we move into the new year, and experts hope the situation in Southwest will not become the norm. Ideally, with boots on the ground and policy experts amidst, enforcement of the Task Force’s recommendations will curb the spread of this threatening epidemic in all areas of the Commonwealth.
References:
[1] Virginia Department of Health. (July 2016). Office of the Chief Medical Examiner Fatal Drug Overdose Quarterly Report, First Quarter 2016. Retrieved from http://www.vdh.virginia.gov/content/uploads/sites/18/2016/04/Quarterly-Drug-Death-Report-FINAL_July-2016.pdf
[2] Lopez, G. (June 2, 2016). The opioid painkiller and heroin epidemic. Retrieved from http://www.vox.com/2015/10/1/9433099/opioid-painkiller-heroin-epidemic
[3] Virginia Department of Health Professions. (April 6, 2015). Governor’s Task Force on Prescription Drug and Heroin Abuse Interim Report. Retrieved from https://www.dhp.virginia.gov/taskforce/minutes/20150512/TaskForceInterimReport05122015.pdf
[4] Center for Disease Control Health Advisory. (October 26, 2015). Increases in Fentanyl Drug Confiscations and Fentanyl-related Overdose Fatalities. Retrieved from https://www.vdh.virginia.gov/OEMS/NewsFeatures/CDCHealthAdvisory-Fentanyl.pdf
[5] Department of Medical Assistance Services. (July 1, 2016). Virginia’s Addiction Treatment Services Delivery System Transformation Concept Paper: 1115 Waiver for Addiction Treatment Services. Retrieved from http://www.dmas.virginia.gov/Content_atchs/bh/VA%20Addiction%20Tx%20Services%20Concept%20Paper-FINAL-7-1-2016.pdf
[6] Partnership News Service. (November 9, 2011). Prescription Opioid Addiction Can Be Treated with Suboxone, Study Shows. Retrieved from http://www.drugfree.org/news-service/prescription-opioid-addiction-can-be-treated-with-suboxone-study-shows/
[7] Ramsey, J. (August 8, 2016). In SW Va., drug to help addicts attacked as part of the problem. Retrieved from http://www.dailyprogress.com/starexponent/news/in-sw-va-drug-to-help-addicts-attacked-as-part/article_d317f8f0-5dc2-11e6-868a-a7b72f83a47b.html.